Chemotherapy
Chemotherapy is a type of cancer treatment that uses drugs to destroy cancer cells.
Chemotherapy works by stopping or slowing the growth of cancer cells, which grow and divide quickly. Sometimes, chemotherapy is used as the only cancer treatment, other times it will be used alongside surgery, radiation therapy, or biological therapy. Chemotherapy can destroy cancer cells that have come back (recurrent cancer) or spread to other parts of your body (metastatic cancer), but it can also harm healthy cells that divide quickly, such as those that line your mouth and intestines or cause your hair and bone marrow to grow. Damage to healthy cells may cause side effects which usually go away after chemotherapy is over.
What does chemotherapy do?
Depending on your type of cancer and how advanced it is, chemotherapy can:
• Cure cancer – when treatment destroys cancer cells to the point that your doctor can no longer detect them in your body and they will not grow back.
• Control cancer – when treatment keeps cancer from spreading, slows its growth, or destroys cancer cells that have spread to other parts of your body.
• Ease cancer symptoms (also called palliative care) – when treatment shrinks tumors that are causing pain or pressure.
How does my doctor decide which chemotherapy drugs to use?
• This will depend on the type of cancer you have. Some types of chemotherapy drugs are used for many types of cancer. Other drugs are used for just one or two types of cancer.
• Whether you have had chemotherapy before
• Whether you have other health problems, such as diabetes or heart disease
How often will I receive chemotherapy?
Treatment schedules for chemotherapy vary widely. How often and how long you get chemotherapy depends on: Your type and stage of cancer, the goals of treatment, the type of chemotherapy and how your body reacts to treatment.
You may receive chemotherapy in cycles. A cycle is a period of treatment followed by a period of rest. For instance, you might receive 1 week of chemotherapy followed by 3 weeks of rest. These 4 weeks make up one cycle. The rest period gives your body a chance to build new healthy cells.
It is not good to skip a treatment but sometimes your doctor or nurse may change your treatment schedule. This can be due to side effects. If this happens, your doctor or nurse will explain what to do and when to start treatment again.
How is chemotherapy given?
• Injection. The medication is given by a shot in a muscle in your arm, thigh, or hip or right under the skin in the fatty part of your arm, leg, or belly.
• Intra-arterial (IA). The medication goes directly into the artery that is feeding the cancer.
• Intraperitoneal (IP). The medication goes directly into the peritoneal cavity (the area that contains organs such as your intestines, stomach, liver, and ovaries).
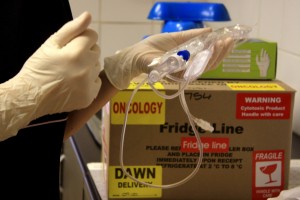
• Intravenous (IV). The medication goes directly into a vein.
• Topically. The medication comes in a cream that you rub onto your skin.
• Orally. The medication comes in pills, capsules, or liquids that you swallow.
Things to know about getting chemo through an IV
Chemotherapy is often given through a needle that is placed in a vein on your hand or lower arm. IV chemotherapy can be administered through catheters or ports, sometimes with the help of a pump.
• Catheters. A catheter is a soft, thin tube. A surgeon places one end of the catheter in a large vein, often in your chest area. The other end of the catheter stays outside your body. Most catheters stay in place until all your chemotherapy treatments are done. Catheters can also be used for drugs other than chemotherapy and to draw blood. Be sure to watch for signs of infection around your catheter.
• Ports. A port is a small, round disc made of plastic or metal that is placed under your skin. A catheter connects the port to a large vein, most often in your chest. Your nurse can insert a needle into your port to give you chemotherapy or draw blood. This needle can be left in place for chemotherapy treatments that are given for more than 1 day. Be sure to watch for signs of infection around your port.
• Pumps. Pumps are often attached to catheters or ports. They control how much and how fast chemotherapy goes into a catheter or port. Pumps can be internal or external. External pumps remain outside your body. Most people can carry these pumps with them. Internal pumps are placed under your skin during surgery.
How will I feel during chemotherapy?
Chemotherapy affects people in different ways. How you feel depends on how healthy you are before treatment, your type of cancer, how advanced it is, the kind of chemotherapy you are getting, and the dose.
The most common side effect of chemotherapy is fatigue. Prepare for fatigue by asking someone to drive you to and from treatments, planning time to rest on the day and the day after treatment, and getting help with chores and childcare.
There are many ways you can help manage side effects. Speak to your doctor or nurse about what you are experiencing and what you can do to ease your side effects.
Can I take over-the-counter and prescription drugs while I get chemotherapy?
This depends on the type of chemotherapy you get and the other types of drugs you plan to take. Take only drugs that are approved by your doctor or nurse. Tell your doctor or nurse about all the over-the-counter and prescription drugs you take, including laxatives, allergy medicines, cold medicines, pain relievers, aspirin, ibuprofen, food supplements and medication from herbalists and traditional healers. These may interact with chemotherapy causing undue effects and reduce the efficacy of the treatment.
Read moreRadiotherapy and Brachytherapy
Radiotherapy uses high-energy rays to treat disease. It can be given both externally and internally. Internal radiotherapy is called brachytherapy.
Radiotherapy works by destroying cancer cells only in the area that’s being treated. Normal cells can also be damaged by radiotherapy, which may cause side effects. Cancer cells cannot repair themselves after radiotherapy, but normal cells usually can.
Ways of giving radiotherapy
There are two ways of giving radiotherapy: external beam radiotherapy (also known as external radiotherapy) and internal radiotherapy.
External radiotherapy aims high-energy x-rays at the affected area using a large machine. Internal radiotherapy involves having radioactive material placed inside the body. This may be a solid radioactive material that is put close to, or inside, the tumor. This is known as brachytherapy. A liquid source of radioactive material called a radioisotope can also be used in internal radiotherapy. This is given as an injection into a vein or taken as an oral liquid or capsule. Whether you have external or internal radiotherapy will depend on the type of cancer you have and where it is in the body. Some cancers are treated with both external and internal radiotherapy.
Possible side effects of Radiotherapy
Side effects may affect you no matter which part of the body you’re having radiotherapy to. It’s important to remember that most people will have side effects and they will often be mild. These include
• Tiredness
• Nausea
• Skin reactions
• Flu-like symptoms
• Hair loss
• Changes in your blood.
• Stomach cramps
• Diarrhea
• Pain when swallowing
There are ways to help you manage side effects so they’re easier to cope with. If you need help and advice about dealing with any, speak to your doctor or radiotherapy staff. Most side effects last for about 10-15 days after treatment finishes.
Some people have side effects that last for longer, or develop a while after they have finished their treatment. These are called long-term or late effects.
Skin markings
Once treatment area has been decided, markings are made on your skin to pinpoint the exact place where the radiation will be directed. Usually, permanent markings are made. They’re the size of a pinpoint and will only be done with your permission. If you have a mould or mask, any marks that need to be made will be made on the mould or mask rather than your skin.
Skin care moulds and masks
To help you stay still and in the same position during daily radiotherapy, you may need to have a mould or mask made before planning starts. This is used to help keep you still so that the treatment is accurate and as effective as possible.
Moulds and masks are commonly used for children having radiotherapy.
How should I prepare for radiotherapy?
Before you start radiotherapy, your clinical oncologist or specialist radiographer will usually arrange an appointment to discuss your treatment and any possible risks or side effects with you.
Radiotherapy can harm a developing baby so you should avoid getting pregnant during treatment. If you think you may be pregnant, speak to your doctor or radiographer immediately. You should also let them know if you have a pacemaker, implantable cardiac device (ICD) or cochlear implant, as these can be affected by radiotherapy.
Radiotherapy may affect how much you can do at home and work. Try to arrange extra help and talk to your employer in advance, to help make it easier to cope.
Pathology Lab
For your convenience, a pathology lab has been set up on site so that you can have all the services available to you from our rooms.
Pathology is the study of disease and helps with diagnosis through the analysis of cells, tissues and bodily fluids. Through pathology, we are able to predict or follow the progression of disease. As a field of general inquiry and research, pathology addresses four components of disease: cause, development, structural alterations of cells (morphologic changes), and the consequences of changes.
Radiology
Radiology is a medical specialty that uses imaging to diagnose and treat diseases seen within the body. Radiologists use a variety of imaging techniques such as X-ray, ultrasound, computed tomography (CT), nuclear medicine including positron emission tomography (PET), Mammography, and magnetic resonance imaging (MRI) to diagnose and/or treat diseases.
Clinical trials -are they an option for me
Advances in oncology can only be made by testing the safety and efficacy of new drugs in people. Cancer clinical trials test new treatments for people with cancer. These can be studies of new types of chemotherapy, other types of treatment, or new ways to combine treatments. The goal of all these clinical trials is to find better ways to help treat you and future generations.
All clinical trials offer quality cancer care. Ask how this clinical trial could help you or others. For instance, you may be one of the first people to get a new treatment or drug. Payment for trials is covered by the company researching the treatment that is part of a clinical trial. Read more about trials on our Stay Up To Date page.
Payment Structure
It is important to talk with your medical scheme before you commence with treatment. Questions to include are:
• What will my insurance pay for?
o Radiological Studies
o Blood tests
o Motivation letters
o Do I need a written referral to see a specialist?
o Scripts
o Medical certificates
o Home nursing
o Home oxygen
• Which hospitals are covered by my plan?
• Benefits following active treatment
• Co-payments
Please note, your first consult with the doctor will be charged to you. A statement will be printed out and this can be used to claim back from your medical aid once registration has been complete. During your treatment, your consults will be charged to your medical aid but once your treatment is complete, the responsibility will be yours to cover consultation fees and claim this back from your medical aid.
How can I best work with my medical aid?
• Read your insurance policy before treatment starts to find out what your plan will and will not pay for.
• Keep records of all your treatment costs and insurance claims.
• Send your insurance company all the paperwork it asks for. This may include receipts from doctors’ visits, prescriptions, and lab work. Be sure to also keep copies for your own records.
• As needed, ask for help with the insurance paperwork.